When To Visit a Cardiologist for Chest Pain Treatment

According to the Centers for Disease Control and Prevention, heart disease is the leading cause of death for adults in the United States. Therefore seeking chest pain treatment is crucial, especially for those at high risk for heart disease. However, chest pain can result from various health issues, so how does one know when it is time to see a cardiologist about it? The following offers advice on when to see a cardiologist for chest pain treatment.
When is chest pain an emergency?
First, it is important to discuss when chest pain is a sign of an emergency like a heart attack. If the chest pain is severe and comes with shortness of breath, racing heartbeat, dizziness, cold sweats, or nausea, this could be a heart attack, and it is time to call 911 or get to the nearest emergency room. However, symptoms of heart attacks and other emergency cardiac events can look different in different people. For example, men may feel numbness and pain on the left arm or side of the chest, while women may experience this on the right. As a rule, it is always better to err on the side of caution and get help immediately if you feel that life or limb is threatened.
When to see a cardiologist about chest pain treatment?
This can be a tricky question to answer because so many things can be behind chest pain. In addition to the symptoms mentioned above, an abnormally slow heart rate, swelling in the legs, burning tightness, or fullness in the chest can also be signs of cardiac issues. However, according to the Cleveland Clinic, chest pain accompanied by the following is less likely to be a cardiac issue:
- A sour taste or a sensation of food re-entering the mouth
- Difficulty swallowing
- Pain that gets better or worse changing position
- Pain that worsens when breathing deeply or coughing
- Tenderness when pressing on one's chest
- Pain lasting for many hours
Conditions such as kidney disease and problems with the lungs or the gastrointestinal system can sometimes be mistaken for cardiac issues.
Patients should consider their symptoms along with their risk factors for heart disease. If a patient has chest pain and other signs of cardiac trouble accompanied by risk factors, they should consider seeing a cardiologist. These risk factors include a family history of heart disease, high blood pressure, diabetes, obesity, high cholesterol, or a sedentary lifestyle. Many patients find it easier to start by talking to their primary care doctor, who can provide them with a referral.
How can a cardiologist help?
In addition to reviewing a patient's medical history and symptoms, a cardiologist can run a number of tests to explore the nature of chest pain and suggest a possible treatment plan. Possible tests include:
- Stress test. Tests to see how the heart responds during exercise or when working hard
- Coronary catheterization. To help look for blockages in the arteries
- CT Scans and MRIs. To look for blockages or to see how blood is flowing through the heart
- Electrocardiogram. A test to measure electrical activity in the heart
- Echocardiogram. A test to check how chambers and valves of the heart are pumping blood
Depending on what the cardiologist finds, they may recommend a course of treatment involving lifestyle changes and medications. Surgery is another possibility if the reason behind the chest pain is something more serious.
Do not ignore signs of cardiac trouble
Chest pain can signal a serious cardiac issue. It is important to seek the help of a medical professional to find out the reason behind it. A cardiologist can help discover why you are having chest pain and get you the treatment you need. To learn more about chest pain treatment and how a cardiologist can help, call our team today.
Request an appointment here: https://boyntonbeach.floridapremiercardio.com or call Florida Premier Cardiology at (561) 229-1411 for an appointment in our Downey office.
Check out what others are saying about our services on Yelp: Chest Pain Treatment in Boynton Beach, FL.
Recent Posts
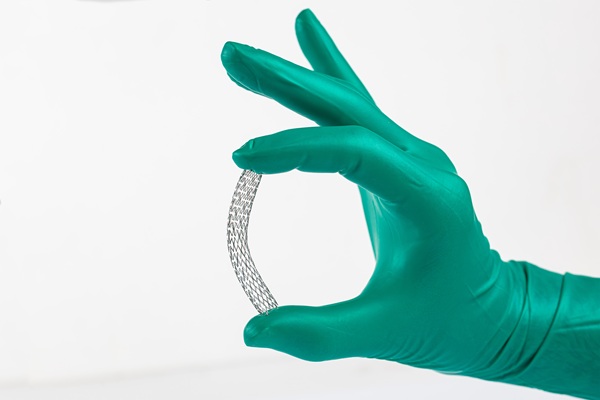
Coronary stent placement is a treatment for coronary artery disease, a buildup of plaque (fat and cholesterol) around the heart's arteries. Along with angioplasty, a stent helps restore blood flow to the heart, relieving symptoms such as chest pain and shortness of breath and helping prevent a heart attack. The following overview of coronary stent…
Heart disease treatment encompasses a range of interventions, from lifestyle changes and medications to surgical interventions. Individuals can manage their condition and improve their quality of life by working with a cardiologist. Successful heart disease treatment starts with the patient having the information they need to make informed decisions about their health.Also known as cardiovascular…
A heart specialist is a doctor specializing in diagnosing and treating cardiovascular conditions. Patients may be referred to one of these doctors for several reasons, from diagnosing a heart health issue to getting cleared for surgery. However, seeing a heart specialist is even more crucial for those either experiencing the signs of heart disease or…
Cardiologists perform angioplasty to open blocked arteries, specifically those caused by coronary disease. This minimally invasive alternative to open heart surgery can restore proper blood flow to the heart and often reverse the fast track to a heart attack. However, learning when one is necessary is crucial for treatment success.Coronary artery disease (CAD) is a…