Peripheral Arterial Disease Symptoms and Treatment Options

Peripheral arterial disease affects blood flow in the arteries, most commonly in the legs. It develops due to plaque buildup in the arteries that causes them to narrow and restrict circulation, possibly leading to discomfort, difficulty walking, and other serious complications. Recognizing the symptoms early and exploring treatment options can help improve the quality of life and reduce the risk of further complications.
Common symptoms of peripheral arterial disease
This condition often progresses slowly, and symptoms may not appear until the condition becomes severe. One of the most common signs is pain or cramping in the legs while walking or exercising, known as claudication. The pain typically goes away with rest but returns with activity. Other symptoms include:
- Weakness or numbness in the legs
- One leg feels colder than the other
- Sores or wounds that are slow to heal on the feet or toes
- A weak or absent pulse in the legs or feet
- Skin discoloration or shiny skin on the legs
In more advanced stages, individuals may experience pain even while resting. If left untreated, peripheral arterial disease can increase the risk of infections, ulcers, and, in severe cases, tissue death, leading to the need for amputation.
Causes and risk factors
The primary cause of peripheral arterial disease is atherosclerosis, where fatty deposits build up in the arteries. Over time, this buildup can restrict blood flow, making it hard for oxygen and nutrients to reach the limbs. Factors that put patients at higher risk of developing this condition include:
- Smoking
- Diabetes
- High blood pressure
- High cholesterol
- Obesity
- A sedentary lifestyle
If a patient has one or more of these risk factors, they are urged to pay attention to any changes in leg health and discuss these changes with a healthcare professional.
Diagnosis and testing
Early detection of the disease is essential for preventing complications. A healthcare provider may use several methods and tests to diagnose the condition. The ankle-brachial index (ABI) is a simple test that compares blood pressure in the arms and legs to determine if there is reduced circulation. Other diagnostic tools may include an angiography, ultrasound imaging to assess blood flow, and blood tests to check blood sugar and cholesterol.
Treatment options for peripheral arterial disease
Treatment for peripheral arterial disease focuses on improving circulation, relieving symptoms, and preventing further complications. Lifestyle changes that include quitting smoking, eating a healthy diet, and exercising are key to managing the condition and can help slow disease progression. Prescription medication can control blood pressure, cholesterol, and blood sugar levels. Additionally, blood thinners can lower the risk of blood clots and improve circulation.
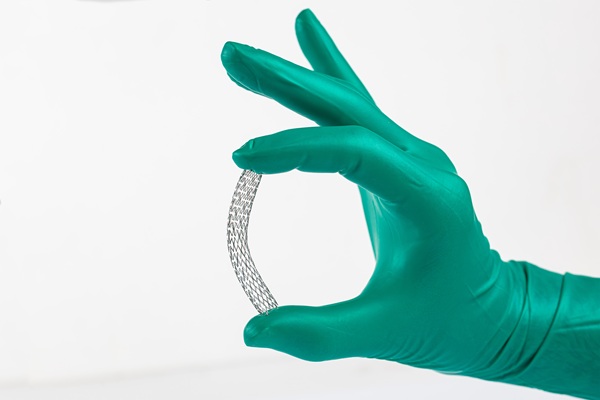
Individuals with severe peripheral arterial disease may need to undergo medical procedures. Angioplasty is a minimally invasive treatment that involves inflating a small balloon in the artery to widen it. In some cases, a stent is placed to keep the artery open. Bypass surgery may be recommended for severe blockages, redirecting blood flow around the affected artery.
Taking steps toward better vascular health
Peripheral arterial disease is a serious condition. However, with early diagnosis and treatment, healthcare providers can help manage symptoms and improve overall vascular health. Those experiencing symptoms should seek medical attention to prevent complications and maintain a better quality of life.
Request an appointment here: https://boyntonbeach.floridapremiercardio.com or call Florida Premier Cardiology at (561) 229-1411 for an appointment in our Boynton Beach office.
Check out what others are saying about our services on Yelp: Peripheral Arterial Disease in Boynton Beach, FL.
Recent Posts
Coronary stent placement is a treatment for coronary artery disease, a buildup of plaque (fat and cholesterol) around the heart's arteries. Along with angioplasty, a stent helps restore blood flow to the heart, relieving symptoms such as chest pain and shortness of breath and helping prevent a heart attack. The following overview of coronary stent…
Heart disease treatment encompasses a range of interventions, from lifestyle changes and medications to surgical interventions. Individuals can manage their condition and improve their quality of life by working with a cardiologist. Successful heart disease treatment starts with the patient having the information they need to make informed decisions about their health.Also known as cardiovascular…
A heart specialist is a doctor specializing in diagnosing and treating cardiovascular conditions. Patients may be referred to one of these doctors for several reasons, from diagnosing a heart health issue to getting cleared for surgery. However, seeing a heart specialist is even more crucial for those either experiencing the signs of heart disease or…
Cardiologists perform angioplasty to open blocked arteries, specifically those caused by coronary disease. This minimally invasive alternative to open heart surgery can restore proper blood flow to the heart and often reverse the fast track to a heart attack. However, learning when one is necessary is crucial for treatment success.Coronary artery disease (CAD) is a…